What Kind of Protocol Is Downregulation IVF?
April 3, 2025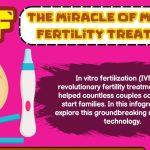
What Does IVF Mean in Medical Terminology?
April 3, 2025How Does IVF Work? A Deep Dive into the Fascinating World of In Vitro Fertilization
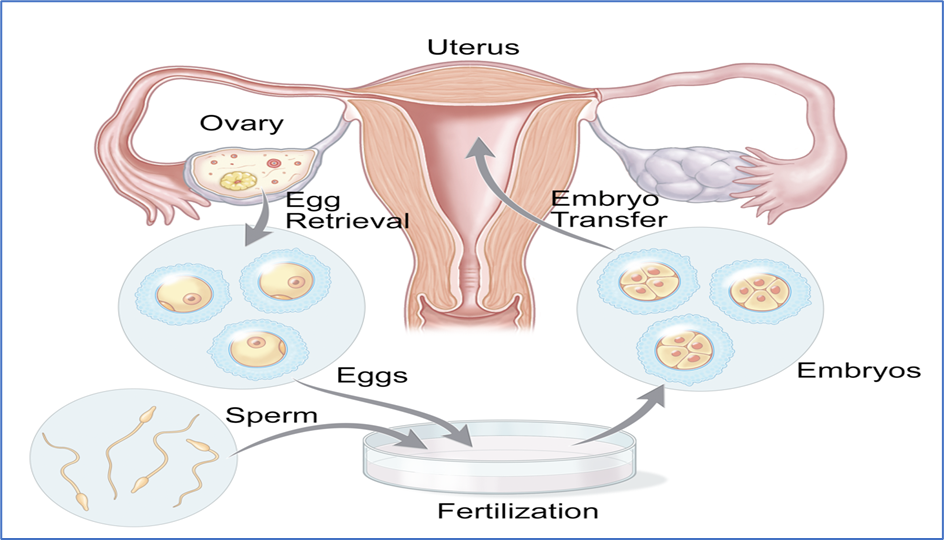
In vitro fertilization, or IVF, might sound like something out of a sci-fi movie—eggs and sperm meeting in a lab dish instead of inside a body—but it’s very real and has helped millions of people start families. If you’ve ever wondered how this process works, you’re not alone! It’s a topic full of surprises, emotions, and even a little bit of magic (well, science that feels like magic). Whether you’re curious about the nitty-gritty details, the behind-the-scenes stuff no one talks about, or just want to know what it’s like for people going through it, this article has you covered.
We’re going to break it all down step by step, sprinkle in some fun facts, and share practical tips that go beyond the basics. Plus, we’ll dig into the latest research and answer questions you didn’t even know you had—like what happens to leftover embryos or how IVF doctors decide which embryo is “the one.” Let’s dive into this incredible journey together!
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is Latin for “in glass.” Basically, it’s a way to help people get pregnant by combining an egg and sperm outside the body, in a lab, and then placing the resulting embryo into the uterus. It’s one of the most common fertility treatments out there, and since the first IVF baby, Louise Brown, was born in 1978, over 8 million babies have come into the world this way. Pretty cool, right?
But IVF isn’t just for one type of person. It’s used by couples struggling with infertility, single parents, same-sex couples, and even people who want to avoid passing on genetic conditions. It’s like a superhero tool in the world of baby-making!
Why Do People Choose IVF?
Here’s where it gets interesting—IVF isn’t always the first thing people try. Some folks turn to it after months or years of trying to conceive naturally. Others jump straight in because of specific challenges, like:
- Blocked fallopian tubes (the highways sperm and eggs use to meet).
- Low sperm count or sluggish swimmers.
- Age-related fertility declines (yep, eggs have an expiration date).
- Unexplained infertility—when doctors shrug and say, “We don’t know why it’s not happening.”
And here’s a fun fact: some people use IVF to pick their baby’s gender or to freeze embryos for later, like a time capsule for future pregnancies. It’s wild to think about, but it’s all part of what makes IVF so fascinating.
Step-by-Step: How IVF Actually Works
IVF isn’t a one-and-done deal—it’s a process with several stages, each one a little like a chapter in a book. Let’s walk through it together, with all the juicy details and some insider scoops you won’t find everywhere else.
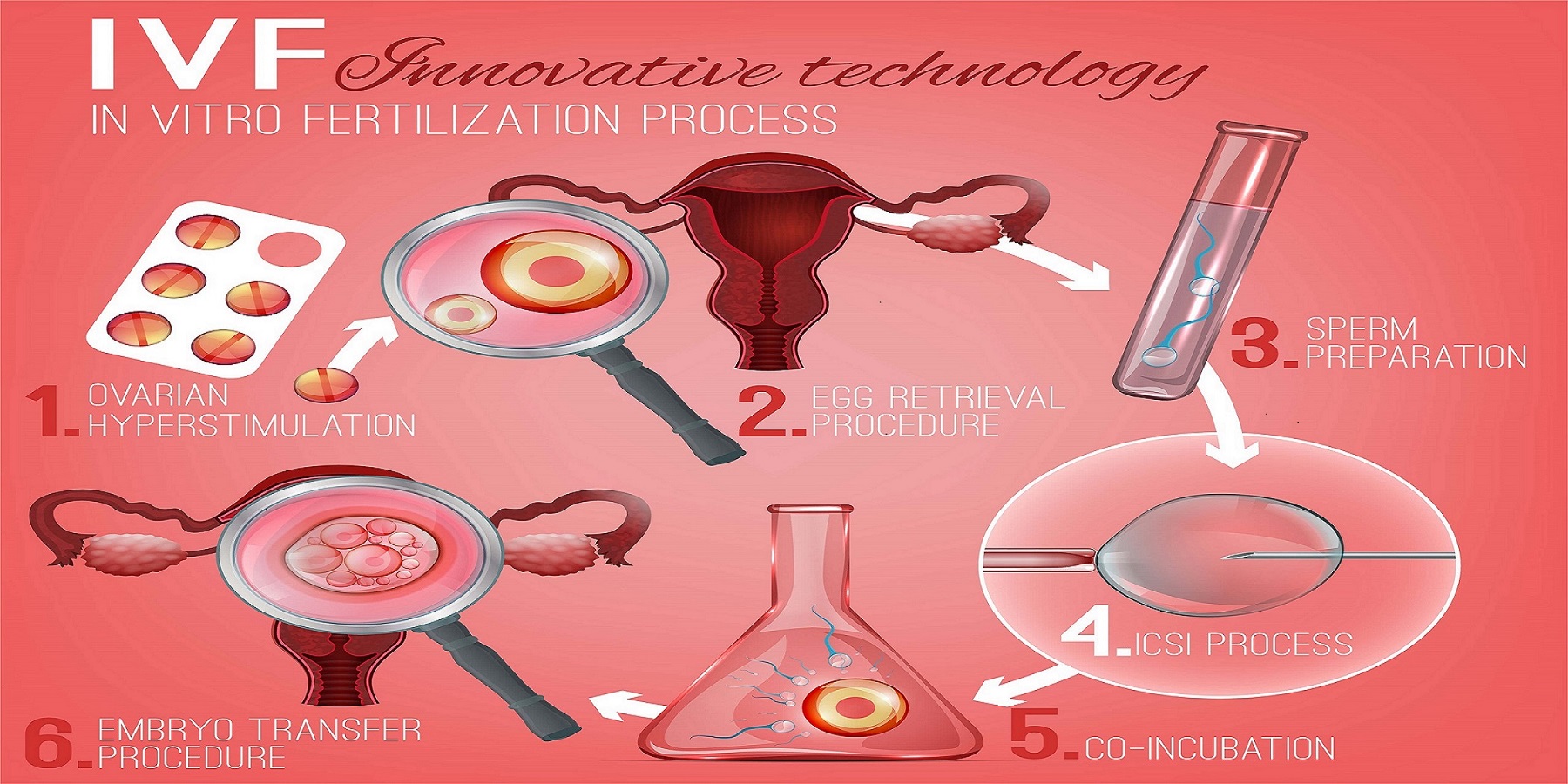
Step 1: Boosting the Ovaries with Hormones
The goal here is to get the ovaries to produce more eggs than usual. Normally, your body releases just one egg a month, but IVF needs a bigger team to work with. So, doctors prescribe hormone injections—like follicle-stimulating hormone (FSH)—to kick things into high gear.
- What it’s like: You’ll give yourself shots at home, usually in your belly or thigh, for about 10-14 days. It’s not as scary as it sounds—think of it like a tiny pinch. Some people even make it a ritual, like a nightly “egg-power-up” session while watching Netflix.
- Fun fact: These hormones can make you feel like you’re on an emotional rollercoaster—happy one minute, teary the next. One mom said, “I cried over a burnt toast during IVF, but it was worth it!”
- Practical tip: ✔️ Keep a calendar to track your shots. ❌ Don’t skip doses—it’s like forgetting to water a plant right when it’s blooming.
Science scoop: A 2023 study from the Journal of Reproductive Medicine found that tweaking hormone doses based on a person’s age and weight can boost egg numbers by up to 20%. Pretty smart, huh?
Step 2: Checking on Those Eggs
While your ovaries are busy, doctors keep an eye on things with ultrasounds and blood tests. They’re looking at how many egg sacs (follicles) are growing and checking hormone levels to make sure everything’s on track.
- What it’s like: You’ll visit the clinic a few times, lying back while a wand-like ultrasound checks your ovaries. It’s not glamorous, but it’s quick.
- Behind the scenes: Nurses often nickname this the “egg watch party.” They’re counting follicles like they’re tallying votes in an election!
- Practical tip: ✔️ Wear comfy clothes to appointments—those paper gowns are chilly. ❌ Don’t stress if numbers fluctuate; it’s normal.
Step 3: The Big Egg Retrieval Day
Once the eggs are ready (usually when follicles hit 18-20 mm), it’s time to get them out. This happens about 36 hours after a final “trigger shot” of a hormone called hCG, which tells the eggs to finish maturing.
- How it works: You’re sedated (no pain!), and a doctor uses a thin needle guided by ultrasound to suck the eggs out of the follicles through your vagina. It takes about 20-30 minutes.
- Wow factor: They can grab 10-15 eggs in one go! That’s like a whole carton from one trip to the ovary store.
- Practical tip: ✔️ Rest afterward—think of it as a Netflix-and-chill day. ❌ Don’t plan anything big; you might feel bloated or crampy.
Dr. Emily Carter, a fertility specialist, says, “Egg retrieval is like a treasure hunt—we’re looking for the best eggs to give you the best shot at a baby.”
Step 4: Sperm Meets Egg in the Lab
Now the magic happens! The eggs go to a lab where they’re mixed with sperm—either from a partner or a donor. There are two ways this can go:
- Traditional IVF: Eggs and sperm are tossed together in a dish, and nature takes its course.
- ICSI (Intracytoplasmic Sperm Injection): A scientist picks one sperm and injects it right into an egg. This is clutch if the sperm need a little help.
- Fun fact: The lab dish isn’t just any old plate—it’s a high-tech petri dish with a special liquid that mimics the body’s environment. Think of it as a VIP lounge for eggs and sperm.
- What people don’t know: Scientists watch the eggs under a microscope for 24 hours to see if they fertilize. It’s like waiting for a text back—nerve-wracking but exciting!
Step 5: Growing Tiny Embryos
Fertilized eggs become embryos, and they’re kept in the lab for 3-5 days to grow. Doctors check them daily, looking at cell division and shape to pick the strongest ones.
- Cool detail: By day 5, an embryo is called a blastocyst—it’s got about 100 cells and looks like a tiny water balloon with a baby-to-be inside.
- Latest research: A 2024 study in Fertility and Sterility showed that AI can now predict which embryos are most likely to succeed with 85% accuracy. Talk about futuristic!
- Practical tip: ✔️ Ask your doctor how many embryos made it—this info helps you plan next steps.
Step 6: The Embryo Transfer
Time to put an embryo (or two) back into the uterus! This is a quick procedure—no sedation needed. A doctor uses a thin tube (catheter) to place the embryo through the cervix.
- What it’s like: It feels like a pap smear—mildly awkward but over fast. You might lie down for 15-30 minutes after to let the embryo settle.
- Secret scoop: Some clinics play calming music during the transfer. One patient said, “I had Beethoven helping my embryo stick!”
- Practical tip: ✔️ Bring a friend for moral support. ❌ Don’t freak out over every twinge—it doesn’t mean success or failure.
Step 7: The Two-Week Wait
Now you wait 9-14 days to take a pregnancy test. This is the hardest part—your embryo is either implanting in the uterus or not, and there’s nothing left to do but hope.
- What people say: “It’s like waiting for the biggest exam results of your life,” one IVF mom shared on a forum.
- Practical tip: ✔️ Distract yourself with hobbies—knitting, gaming, whatever works. ❌ Don’t test early; it can give false results and mess with your head.
What Happens Behind the Scenes?
IVF isn’t just shots and lab dishes—there’s a whole world of stuff going on that most people don’t see. Let’s pull back the curtain!
The Embryo Grading Game
Doctors “grade” embryos based on how they look—size, symmetry, and cell count. It’s like a beauty pageant for tiny cell clusters! A top-grade embryo (like an AA or 5AB) has a better shot at becoming a baby, but even lower grades can work.
- Science bit: A 2023 study found that grade B embryos still led to pregnancies 40% of the time—so don’t count them out!
- Tip: Ask your doctor to explain your embryos’ grades. It’s your backstage pass to the process.
What About Leftovers?
Not all embryos get transferred right away. extras can be frozen for later—think of it like putting a cake in the freezer for a future party. Some people even donate them to other couples or for research.
- Wow moment: Frozen embryos can stay good for decades. A baby was born in 2020 from an embryo frozen in 1992—older than some of you reading this!
- Tip: ✔️ Talk to your clinic about storage fees (usually $500-$1,000 a year). ❌ Don’t ignore the decision—it’s a big one.
The Emotional Side No One Talks About
IVF can be a wild ride—hope, fear, joy, and disappointment all mashed together. Couples say they bond over the weirdest things, like naming their embryos (“Meet Bubbles and Spike!”) or celebrating each step with a special snack.
- Real talk: “I felt like a science experiment, but also like a warrior,” one woman told me. It’s tough, but it builds resilience.
How Successful Is IVF, Really?
Success rates depend on a bunch of things—age, health, and even luck. Here’s a quick breakdown based on 2022 U.S. data from the CDC:
| Age Group | Chance of Live Birth per Cycle |
|---|---|
| Under 35 | 50-55% |
| 35-37 | 40-45% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
- Key takeaway: Younger eggs = better odds. But don’t lose hope—new tricks like genetic testing are bumping up success for older folks.
- Tip: ✔️ Ask your clinic for their success rates—they vary!
Dr. James Patel, a reproductive endocrinologist, notes, “IVF success isn’t just about numbers—it’s about finding the right plan for each person’s unique body.”
Risks and Realities: What to Watch For
IVF is pretty safe, but it’s not risk-free. Here’s what to know:
- Ovarian Hyperstimulation Syndrome (OHSS): Hormones can overstimulate ovaries, causing bloating or pain. Rare but serious cases need a doctor ASAP.
- Multiple Births: Transferring more than one embryo can mean twins or triplets—cute, but riskier for mom and babies.
- Emotional Toll: It’s a marathon, not a sprint. Stress is real, and support groups can be a lifesaver.
Tip: ✔️ Talk to your doctor about single embryo transfers to lower risks. ❌ Don’t bottle up feelings—chat with a counselor if needed.

Costs and Cash-Saving Hacks
IVF isn’t cheap—a cycle in the U.S. averages $12,000-$15,000, plus meds ($3,000-$5,000). Insurance might cover some, but not always. Here’s how to make it work:
- Grants: Groups like Baby Quest offer cash to help.
- Mini IVF: Uses fewer drugs, costs less ($5,000-$7,000), but may need more cycles.
- Shared Risk Programs: Pay upfront for multiple cycles; get a refund if it doesn’t work.
Tip: ✔️ Shop around—clinics have different prices. ❌ Don’t assume you can’t afford it; explore options first.
The Latest IVF Buzz: What’s New in 2025?
IVF keeps evolving! Here’s what’s hot right now:
- AI in Embryo Selection: Machines are helping pick winners, boosting success rates.
- Mitochondrial Donation: Swapping out faulty cell parts to prevent genetic diseases—still experimental but promising.
- At-Home Monitoring: Wearables to track hormones are in testing. Imagine doing IVF with a smartwatch!
Science scoop: A 2024 trial in Nature Medicine showed mitochondrial tweaks could cut miscarriage rates by 15% in some cases. The future is wild!
IVF Myths Busted!
Let’s clear up some confusion:
- Myth: IVF babies are “test-tube freaks.”
Truth: They’re just like any other kid—born from love and science. - Myth: IVF always works on the first try.
Truth: It’s more like a 50/50 shot for younger folks, less as you age. - Myth: It’s only for women.
Truth: Guys with sperm issues are half the equation!
Your IVF Survival Guide
Ready to dive in? Here’s a step-by-step checklist to rock your IVF journey:
- Find a Clinic: Look for good vibes and solid success rates.
- Ask Questions: How many eggs? What’s the plan if it fails?
- Prep Your Body: Eat well, sleep lots, cut stress.
- Build a Team: Friends, family, or a support group—don’t go it alone.
- Celebrate Wins: Every step forward is huge—treat yourself!
Tip from the trenches: “I kept a journal of every shot and ultrasound—it was my IVF scrapbook,” one dad shared. Keeps you sane!
Let’s Talk: What Do You Think?
IVF is a big deal—science, hope, and a dash of mystery all rolled into one. What’s your take? Have you or someone you know gone through it? Drop your thoughts below—I’d love to hear your stories or questions! And if you’re curious about something we didn’t cover, ask away. Let’s keep this conversation going!