
IVF Florida Reproductive Associates: Your Ultimate Guide to Fertility Success
April 11, 2025The IVF Process Timeline: A Step-by-Step Journey to Parenthood
So, you’re thinking about in vitro fertilization (IVF)? Maybe you’ve heard it’s a rollercoaster ride, or perhaps you’re just curious about what really happens behind the scenes. Either way, you’re in the right place! IVF is one of the most incredible ways science helps people become parents, but it’s also a deeply personal journey full of surprises, emotions, and even some quirky details most folks don’t talk about. This isn’t just a dry list of steps—it’s a guide packed with insider scoops, practical tips, and the latest research to help you feel ready, informed, and maybe even a little excited.
We’re going to walk through the entire IVF process timeline, from the moment you decide to start to the day you (hopefully!) hold your baby. Along the way, we’ll uncover hidden gems—like why some people swear by pineapple cores or how a Netflix binge might save your sanity. Plus, we’ll dive into stuff other articles skip, like what the latest studies say about boosting your odds and how to handle the emotional curveballs. Ready? Let’s get started!

What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is just a fancy way of saying “fertilization in a lab.” Picture this: instead of an egg and sperm meeting inside your body like in a classic romance movie, they get together in a petri dish under a scientist’s watchful eye. Then, the resulting embryo is placed back into the uterus to grow into a baby. It’s like giving nature a little high-tech nudge!
IVF has been around since 1978 when the first “test-tube baby,” Louise Brown, was born in England. Since then, it’s helped millions of people—over 8 million babies worldwide, according to recent estimates! It’s not just for couples with infertility, either. Single folks, same-sex couples, and people preserving their fertility for later use it too. But what does the timeline look like? Spoiler: it’s not a quick weekend project—it takes weeks, patience, and a whole lot of hope.
The Big Picture: How Long Does IVF Take?
Before we dive into the nitty-gritty, let’s zoom out. A full IVF cycle—from the first hormone shot to the pregnancy test—usually takes 4 to 6 weeks. But that’s just one “cycle,” and many people need more than one to succeed. Add in prep time, consultations, and recovery, and you’re looking at 2 to 3 months for the whole shebang, assuming everything goes smoothly. Here’s a quick breakdown:
- Prep Phase: 2-4 weeks (consultations, tests, planning)
- Active Cycle: 4-6 weeks (medications, egg retrieval, embryo transfer)
- Waiting Game: 9-14 days (to test for pregnancy)
But here’s the catch: every step has its own mini-timeline, and things like your age, health, or even a random cold can stretch it out. Let’s break it down step by step so you know exactly what to expect.
Step 1: Getting Ready for IVF (Weeks 1-4)
What’s Happening?
This is the “behind-the-scenes” phase where you and your doctor set the stage. Think of it like prepping for a big play—costumes, rehearsals, and all. You’ll meet with a fertility specialist, get some tests done, and figure out a game plan tailored just for you.
The Details
- Consultation: You’ll spill your story—how long you’ve been trying, your medical history, even your coffee habits (yep, they might ask!). The doctor will explain IVF, risks, and costs (spoiler: it’s not cheap—about $15,000 per cycle in the U.S. on average).
- Tests: Bloodwork checks your hormone levels (like FSH and AMH), ultrasounds peek at your ovaries, and your partner might get a sperm analysis. Fun fact: some clinics even test your vitamin D levels—low levels can mess with success rates!
- Custom Plan: Based on your results, the doc picks a protocol. Are you a “long protocol” person (more prep time) or a “short protocol” one (faster start)? It’s all about your body’s quirks.
Insider Scoop
Ever wonder what doctors don’t tell you upfront? A lot of people secretly stress about their “ovarian reserve”—the number of eggs you’ve got left. One patient I heard about kept a journal of her dreams during this phase (she swore they got weirder!). And here’s a quirky tip: some folks start eating Brazil nuts for selenium—there’s no hard proof it helps, but it’s a fan favorite in IVF forums.
Research Boost
A 2023 study from the American Society for Reproductive Medicine found that women with higher vitamin D levels had a 10% better chance of a successful embryo transfer. So, maybe sneak in some sunshine or a supplement?
Practical Tips
✔️ Do: Ask your doctor, “What’s my egg count like?” It’s your body—own the info!
❌ Don’t: Panic if your numbers aren’t “perfect”—IVF can work with just a few good eggs.
✔️ Try: A relaxing hobby (knitting, anyone?) to keep your mind off the waiting.
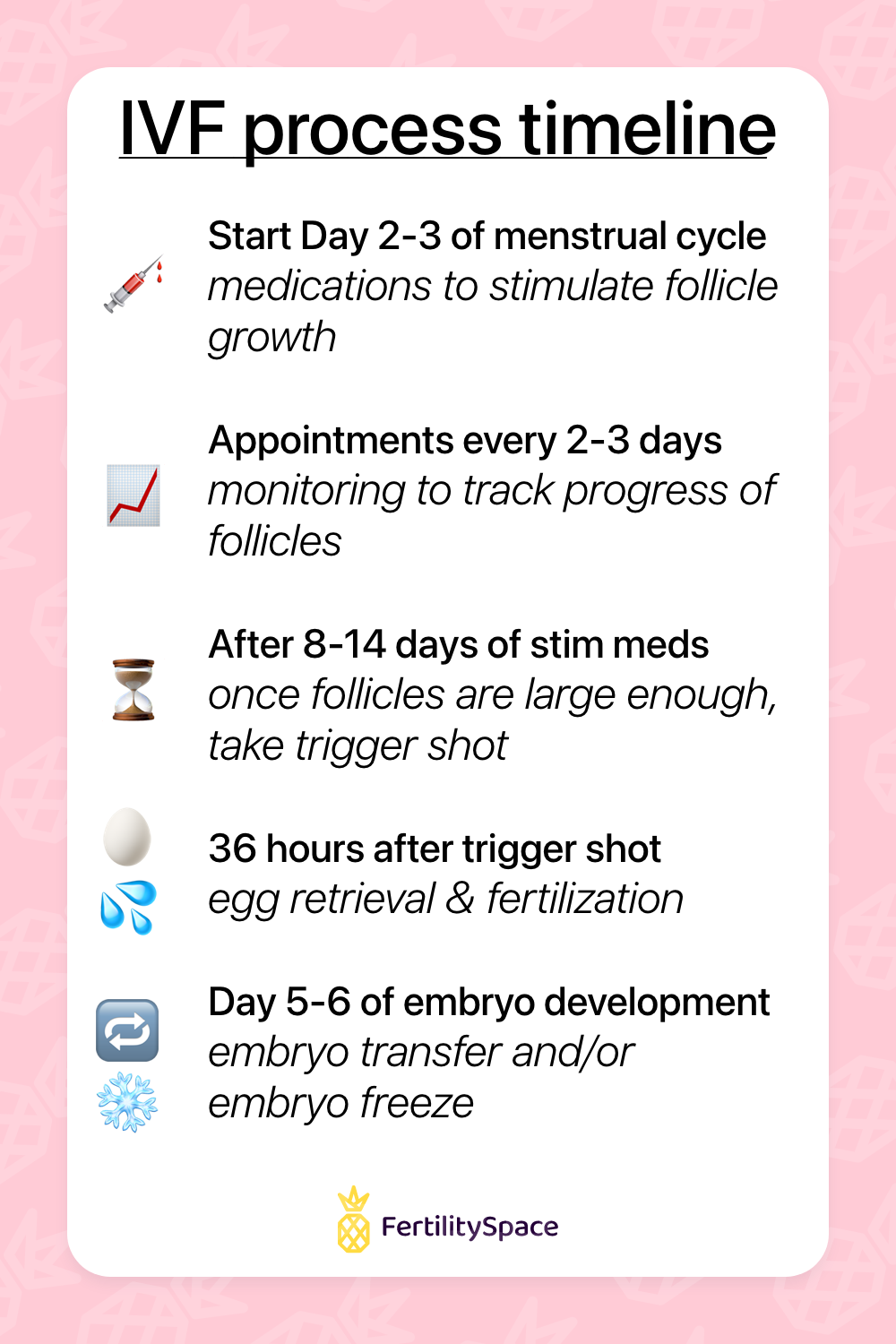
Step 2: Boosting Your Eggs (Days 1-14 of the Cycle)
What’s Happening?
Now the action starts! Your ovaries usually pop out one egg a month, but IVF needs a squad. You’ll take hormone meds to wake up more eggs—like calling in the backups for a big game.
The Details
- Day 1: Your period starts—that’s the official kickoff. You might begin with birth control pills (weird, right?) to sync your cycle or jump straight to injections.
- Days 2-10: Daily shots of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) tell your ovaries, “Let’s make more eggs!” You’ll visit the clinic every few days for ultrasounds and blood tests to track growth.
- Trigger Shot: Around Day 12-14, when your eggs are ready (follicles about 18-20mm), you get a final shot of hCG or a GnRH agonist to ripen them up.
Insider Scoop
Here’s where it gets real: those shots? You might give them to yourself in the belly or thigh. One woman said she felt like a “human pincushion” but got so good she could do it while watching Stranger Things. And the bloating—oh, the bloating! Some call it the “IVF muffin top.” Pro tip: loose pants are your new BFF.
Research Boost
A 2024 study in Fertility and Sterility showed that adding a low dose of letrozole (a breast cancer drug) to FSH can boost egg numbers in women over 35 without extra side effects. Cool, huh?
Practical Tips
✔️ Do: Set a phone alarm for your shots—consistency is key.
❌ Don’t: Skip clinic visits, even if you’re tired of the waiting room magazines.
✔️ Try: Eating pineapple core (it’s got bromelain, which some swear helps implantation—science is iffy, but it’s tasty!).
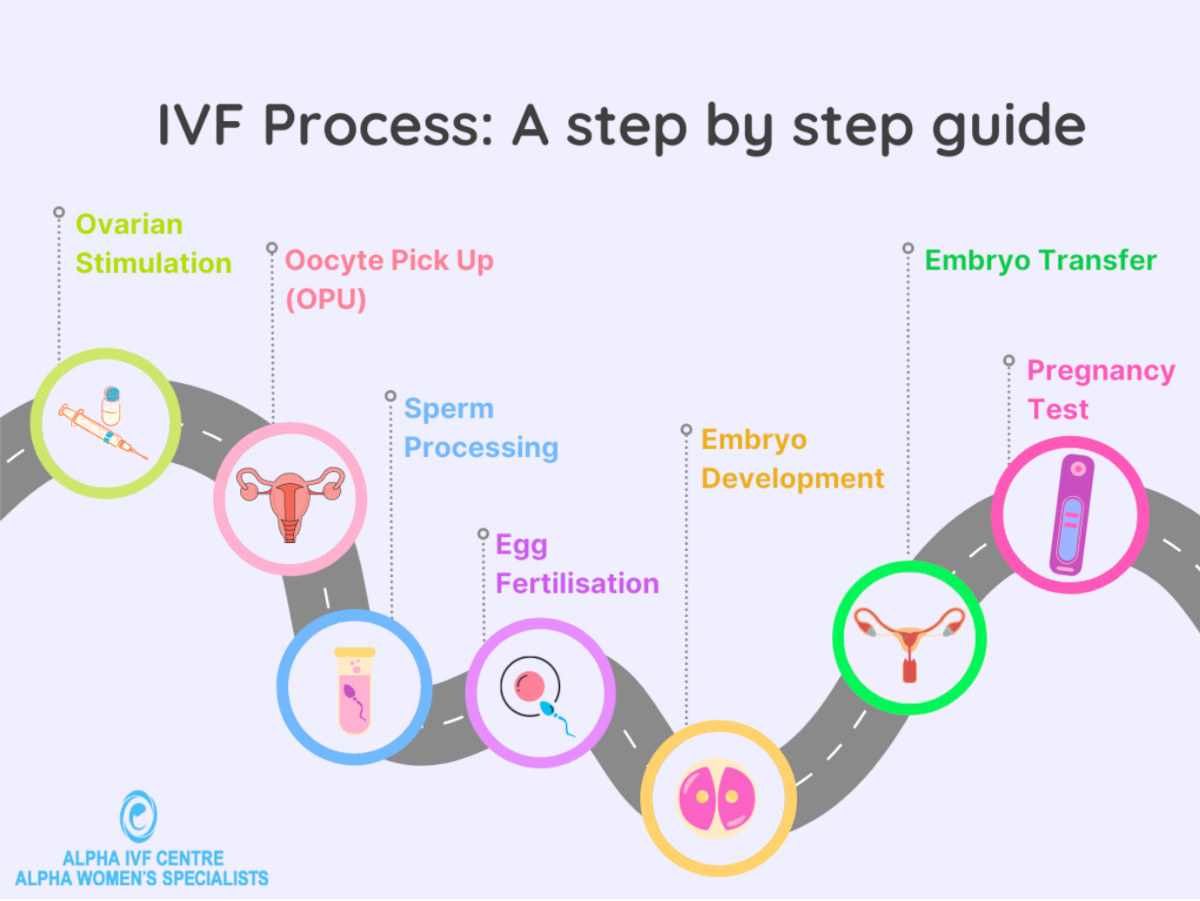
Step 3: Egg Retrieval Day (Day 14-16)
What’s Happening?
It’s showtime! About 36 hours after your trigger shot, you’ll head to the clinic to get those eggs out. This is a quick procedure, but it’s a big deal.
The Details
- The Process: You’re sedated (no pain, just sleep), and the doctor uses an ultrasound-guided needle through your vagina to suck out the eggs. It takes 20-30 minutes.
- Egg Count: They aim for 8-15 eggs, but it varies. One egg? Still a chance. 20? Awesome, but not too many (to avoid complications).
- Aftermath: You’ll rest for an hour, then head home. Expect cramps and maybe spotting.
Insider Scoop
Here’s a secret: some people get weirdly attached to their egg count. “I got 12!” one friend bragged like it was a high score. Also, your partner’s in the spotlight too—they’ll give a sperm sample the same day (or use frozen/donor sperm). One couple I know turned it into a “date” with coffee afterward—cute, right?
Expert Quote
Dr. Emre Seli from Yale Medicine says, “Egg retrieval is a turning point—patients often feel a mix of relief and nerves, but it’s where hope starts to take shape.”
Practical Tips
✔️ Do: Bring a cozy blanket—clinics can be chilly!
❌ Don’t: Plan a big day after—you’ll want to nap.
✔️ Try: Asking, “How’d my eggs look?” It’s okay to be curious!
Step 4: Fertilization and Embryo Growth (Days 16-21)
What’s Happening?
Your eggs meet the sperm in the lab—think of it as a science-y blind date. Then, the embryos grow for a few days while the team watches them like proud parents.
The Details
- Fertilization: Eggs and sperm mix naturally, or they use ICSI (intracytoplasmic sperm injection), where one sperm is injected into each egg. Success rate? About 60-80% fertilize.
- Embryo Culture: For 3-5 days, embryos grow in a special incubator. By Day 5, the best ones reach the blastocyst stage—ready for transfer.
- Updates: You’ll get calls like, “Six fertilized!” or “Three made it to blastocyst!”—it’s a nail-biter.
Insider Scoop
Ever heard of “embryo nicknames”? Some people name them—like “Blasty” or “Little Nugget”—to feel connected. And the lab? It’s not all serious—rumor has it some embryologists play classical music for the embryos (no proof it helps, but it’s adorable).
Research Boost
A 2023 study found that time-lapse imaging (watching embryos grow 24/7) can pick winners 15% better than old-school methods. More clinics are jumping on this tech train.
Practical Tips
✔️ Do: Ask for updates—it’s your journey!
❌ Don’t: Google every embryo milestone—you’ll drive yourself nuts.
✔️ Try: A mini-celebration (cupcake, anyone?) for making it this far.
Step 5: Embryo Transfer (Day 21-23)
What’s Happening?
Time to put the embryo(s) back where they belong—in your uterus! It’s quick, painless, and a huge milestone.
The Details
- Fresh or Frozen: Some do a “fresh” transfer 3-5 days after retrieval; others freeze embryos and transfer later (better odds for some).
- The Procedure: You’re awake, legs up, and the doctor slides a catheter through your cervix to place the embryo. Takes 10 minutes.
- How Many?: Usually one embryo for women under 37 to avoid twins; older folks might get two.
Insider Scoop
Your bladder needs to be full for this—yep, you’ll be squirming! One woman said she sang Baby Shark in her head to stay calm. And after? You’re not “bedridden”—despite what Aunt Karen says, light activity is fine.
Expert Quote
Dr. Jane Frederick, a fertility specialist, notes, “The transfer is simple, but the emotional weight is huge—patients often say it’s when they feel closest to their dream.”
Practical Tips
✔️ Do: Wear comfy socks—your feet will be in stirrups.
❌ Don’t: Chug water last-minute; sip steadily an hour before.
✔️ Try: Visualizing your embryo “sticking”—it’s a mental hug.
Step 6: The Two-Week Wait (Days 23-37)
What’s Happening?
Now you wait—9 to 14 days—to see if the embryo implants and you’re pregnant. It’s the longest two weeks ever.
The Details
- What’s Going On: The embryo burrows into your uterine lining (implantation). You might take progesterone (pills, shots, or suppositories) to help.
- Symptoms: Maybe cramps, spotting, or nada—it’s a guessing game.
- Test Day: A blood test checks hCG levels (the pregnancy hormone). Home tests? Tempting, but wait for the official word.
Insider Scoop
This is when people go wild with superstitions—wearing lucky socks, eating pomegranate seeds, or avoiding cold drinks. One forum swears by “couch potato mode,” but studies say normal life is okay. Netflix binges? Highly recommended.
Research Boost
A 2024 study in Reproductive BioMedicine Online found that stress during the wait doesn’t lower success rates—huge relief, right? Focus on chilling out.
Practical Tips
✔️ Do: Plan distractions—movies, puzzles, whatever works.
❌ Don’t: Test early—it’s a rollercoaster you don’t need.
✔️ Try: Journaling your feelings—it’s cheaper than therapy!
Step 7: The Pregnancy Test and Beyond (Day 37+)
What’s Happening?
The moment of truth—a blood test tells you if you’re pregnant. If yes, congrats! If not, it’s time to regroup.
The Details
- Positive Result: HCG over 25 mIU/mL means pregnant! You’ll get ultrasounds at 6-8 weeks to check the heartbeat.
- Negative Result: It stinks, but 50-60% of first cycles fail. You can try again—many succeed on round two or three.
- Next Steps: Pregnant? Prenatal care kicks in. Not pregnant? Meet your doc to tweak the plan.
Insider Scoop
A positive test doesn’t always sink in—one mom-to-be said she stared at her result for 10 minutes, then ate ice cream to celebrate. Negative? People often hide their grief—reach out to a support group; you’re not alone.
Expert Quote
Dr. Aimee Eyvazzadeh, the “Egg Whisperer,” says, “A negative test isn’t the end—it’s data. We learn, adjust, and keep going.”
Practical Tips
✔️ Do: Have a plan for both outcomes—treat yourself either way.
❌ Don’t: Blame yourself—biology’s tricky, not your fault.
✔️ Try: Talking to someone who’s been there—it’s gold.
What Affects the IVF Timeline?
The 4-6 week cycle sounds neat, but life’s messy. Here’s what can stretch or shrink it:
- Age: Under 35? Higher success, fewer cycles. Over 40? Might need more tries.
- Health: PCOS, endometriosis, or low sperm count can complicate things.
- Clinic Delays: Busy schedules or lab hiccups might push dates.
- Response: Some ovaries are sleepy—meds get adjusted, adding time.
Fun Fact: One couple’s retrieval got delayed because of a snowstorm—nature loves a plot twist!
Boosting Your Odds: Latest Tricks and Tips
Want to stack the deck? Here’s what’s hot in IVF land:
- Preimplantation Genetic Testing (PGT): Screens embryos for chromosomal issues—ups live birth rates by 20% for women over 37 (2023 data).
- Frozen Transfers: Freezing all embryos and transferring later cuts risks like OHSS (ovarian hyperstimulation syndrome) and boosts success by 10-15%.
- Lifestyle Hacks: Ditch smoking (duh), cut caffeine to 1 cup/day, and aim for a BMI of 19-30—studies link these to better outcomes.
Weird but True: Acupuncture during IVF? A 2024 meta-analysis found it might bump success rates by 8%. Worth a shot (or a needle)!
The Emotional Side: What No One Tells You
IVF isn’t just shots and scans—it’s a feelings fest. Here’s the real talk:
- Highs: Seeing your embryos? Magical. Positive test? Tears of joy.
- Lows: Negative results sting. Hormones make you cry at dog food ads.
- Couple Stuff: Some grow closer; others bicker over who forgot the meds.
Pro Tip: One woman kept a “hope jar”—wrote down good moments to read when she felt down. Steal that idea!
Costs and Coverage: The Money Talk
IVF’s pricey—$12,000-$20,000 per cycle, plus meds ($3,000-$5,000). Insurance? Spotty—only 19 U.S. states mandate some coverage. Tips:
- Grants: Look into Resolve.org for options.
- Clinics: Some offer refunds if it fails—ask!
- Savings: Start a “baby fund” early.
Fun Fact: One couple sold old Pokémon cards to fund their cycle—creative!
When IVF Doesn’t Work: What’s Next?
About half of first cycles fail, but don’t lose hope. Options:
- Try Again: Success jumps to 70% by cycle three.
- Donor Eggs/Sperm: Higher odds if age or quality’s the issue.
- Surrogacy: If your uterus says no, someone else can step in.
Real Story: After three fails, one woman switched to donor eggs and had twins—proof there’s more than one path.
The Future of IVF: What’s Coming?
IVF’s evolving fast. Check this out:
- AI: Predicting embryo success with 90% accuracy (2024 trials).
- In Vitro Gametogenesis (IVG): Making eggs/sperm from skin cells—still experimental, but wild!
- Affordability: Mini-IVF (fewer drugs, lower cost) is gaining traction.
Prediction: By 2030, IVF might be as common as braces—accessible and routine.
Your IVF Survival Kit
Here’s your cheat sheet to rock this journey:
- Gear: Heating pad (cramps), comfy clothes, a good playlist.
- Support: Friends, a therapist, or online groups (HealthUnlocked’s great).
- Mindset: Celebrate small wins—every step counts.
Random Gem: One patient swore her lucky unicorn slippers got her through—find your talisman!
Let’s Chat: Your Turn!
You’ve made it through the IVF timeline—phew! What’s on your mind? Drop a comment below:
- What step are you most curious about?
- Got a quirky IVF tip to share?
- How do you stay sane during the wait?
Let’s build a little community right here—your story might just help someone else. And hey, if you’re starting soon, good luck—you’ve got this!
