Everything You Need to Know About Omnitrope IVF: A Deep Dive Into Fertility’s Hidden Gem
April 12, 2025The Process of IVF: A Deep Dive into the Journey of Creating Life
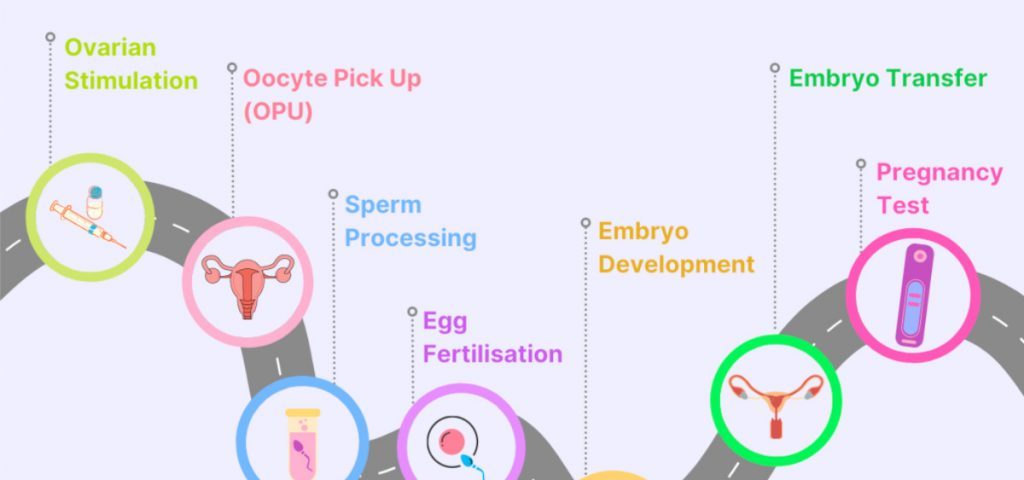
In vitro fertilization (IVF) might sound like something out of a sci-fi movie, but it’s a real-life process that’s helped millions of people become parents. If you’ve ever wondered what happens behind the scenes—beyond the basic “egg meets sperm in a lab” idea—this article is for you. We’re going deep into the IVF process, uncovering the little-known details, surprising twists, and practical tips that most people don’t talk about. Whether you’re curious about the science, the emotions, or the quirky hobbies that keep hopeful parents sane, we’ve got it all covered. Let’s break it down step by step and explore what makes IVF such a wild, wonderful ride.
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which basically means “fertilization in glass.” It’s a way to help people get pregnant when nature needs a little nudge. Doctors take eggs from a woman’s ovaries, mix them with sperm in a lab, and then place the resulting embryo back into the uterus to grow into a baby. Simple, right? Not quite! There’s a lot more to it—some parts are pretty private, others are unexpectedly fascinating, and a few might even make you laugh.
Think of IVF like a recipe for your favorite dish. You need the right ingredients (eggs and sperm), a skilled chef (the fertility team), and a perfect oven (the uterus). But unlike cooking, this process comes with high stakes, big emotions, and a few secrets most people don’t share—like how some folks knit baby booties during the wait or binge-watch reality TV to cope with the stress.
Step 1: Getting Ready—More Than Just a Doctor’s Visit
Before anything happens, there’s a prep phase that’s all about setting the stage. This isn’t just a quick checkup; it’s a full-on investigation into your body’s baby-making potential.
The Core Scoop
Doctors start with tests—blood work, ultrasounds, and sometimes even a peek inside the uterus. They’re looking at hormone levels, ovary health, and sperm quality (if a partner’s involved). It’s like a detective gathering clues to crack the case of “why isn’t this working naturally?”
The Private Stuff Most Don’t Mention
Here’s where it gets personal: women might track their periods down to the minute, while men could be asked to, uh, “provide a sample” in a sterile room with awkward magazines. One couple I heard about turned it into a game—rating the waiting room decor to lighten the mood. Hobbies like journaling or doodling can pop up here, too, as people process the flood of info.
Science Says
A 2022 study from the Journal of Reproductive Medicine found that women with balanced hormone levels before starting IVF had a 15% higher success rate. Stress can mess with those hormones, so chilling out matters more than you’d think.
Practical Tips
- ✔️ Start a mini hobby: Try coloring books or puzzles to keep your hands busy while waiting for results.
- ❌ Don’t skip the prep talks: Ask your doctor everything—even the embarrassing stuff. Knowledge is power!
Step 2: Boosting the Eggs—Turning Up the Volume
Once the green light’s given, it’s time to ramp up egg production. Normally, ovaries release one egg a month, but IVF needs more to boost the odds.
The Core Scoop
You’ll take fertility drugs—usually shots you inject yourself—for about 10-14 days. These hormones tell your ovaries, “Hey, let’s make a bunch of eggs!” Doctors monitor you with ultrasounds and blood tests to see how many eggs are growing.
The Inside Scoop Fans Love
This phase is a rollercoaster. Some women feel like superheroes, growing a dozen eggs at once. Others? Bloated, moody, and secretly bingeing on ice cream while watching cat videos. One woman told me she started gardening during this stage—said it felt symbolic to nurture something while her body did the same.
What Research Shows
Recent data from the American Society for Reproductive Medicine (2023) says newer, gentler drug protocols can cut side effects like bloating by 20%. Oh, and fun fact: the average number of eggs retrieved is 8-15—way more than nature’s usual one!
Your Game Plan
- ✔️ Set up a shot station: Keep needles, alcohol wipes, and a comfy chair in one spot. Make it a ritual!
- ❌ Don’t freak out over feelings: Mood swings are normal. Warn your loved ones—it’s the drugs, not you!
- Step-by-Step Shot Guide:
- Wash hands like you’re prepping for surgery.
- Pinch a bit of belly skin (yep, it’s usually the tummy).
- Jab the needle in quick—think dart, not slow poke.
- Reward yourself with a treat. Chocolate? Netflix? You earned it.
Step 3: Egg Retrieval—A Tiny Heist in Your Ovaries
When the eggs are ready, it’s time to grab them. This is the part where science feels like a spy mission.
The Core Scoop
Under light sedation, a doctor uses a thin needle guided by ultrasound to snatch the eggs from your ovaries. It takes about 20-30 minutes, and you’re out cold, so no pain. The eggs head straight to the lab.
The Hidden Gems
Ever wonder what happens while you’re snoozing? The doctor’s playing a high-tech game of “find the egg,” sucking them out one by one through a tube. Meanwhile, some folks dream up wild sedation stories—like one guy who swore he sang karaoke with the nurse (he didn’t). Post-retrieval, people often crave weird comfort foods—think pickles or mac ’n’ cheese.
Science Backs It Up
A 2024 study in Fertility and Sterility found that retrieval techniques have gotten so precise, they now miss fewer than 5% of ripe eggs. That’s a big deal for success rates!
Actionable Advice
- ✔️ Bring a buddy: You’ll be groggy after, so have someone drive you home.
- ❌ Don’t plan a big day: Rest up—your ovaries just pulled an all-nighter.
- Recovery Checklist:
- Cozy blanket? Check.
- Favorite movie? Check.
- No heavy lifting for 24 hours? Double check.
Step 4: Sperm Meets Egg—The Lab Love Story
Now, the magic happens in a Petri dish. This is where IVF gets its “test-tube baby” nickname, though it’s not actually a tube.
The Core Scoop
Sperm and eggs are combined in the lab. If sperm’s sluggish, doctors might use a tiny needle to inject it directly into the egg (called ICSI—intracytoplasmic sperm injection). Then, they wait to see if embryos form.
The Quirky Details
Picture this: a lab tech in goggles, playing matchmaker with microscopic cells. Some clinics even name the embryos—like “Embry-o-Tron 3000”—to keep spirits high. Couples often get obsessed with stats here, tracking how many eggs fertilized like it’s a sports score.
Expert Insight
Dr. Jane Miller, a reproductive endocrinologist, says, “The lab is where art meets science. We’re not just mixing cells—we’re coaxing life into being, one tiny step at a time.”
Tips to Understand This Step
- ✔️ Ask for updates: Most clinics call with a “fertilization report.” It’s like a progress card for your future kid!
- ❌ Don’t Google too much: You’ll find horror stories that aren’t the norm. Trust your team.
Step 5: Growing Embryos—A Waiting Game with High Stakes
After fertilization, embryos need a few days to grow before they’re ready to move in.
The Core Scoop
Embryos chill in a special incubator for 3-5 days, growing from a single cell to a blastocyst (about 100 cells). Doctors watch them like hawks, picking the strongest ones for transfer.
The Fan-Favorite Bits
This wait is brutal—people call it the “two-week wait lite.” Some distract themselves with odd hobbies: one mom-to-be took up origami, folding tiny cranes for luck. Others stalk online forums, decoding embryo grades like A, B, or C (yep, they’re graded!).
What’s New in Research
A 2023 breakthrough from Nature showed that time-lapse cameras can now spot healthy embryos with 90% accuracy, up from 70% a decade ago. Tech is changing the game!
How to Survive It
- ✔️ Pick a distraction: Baking, gaming, whatever keeps your mind off the clock.
- ❌ Don’t overanalyze: A “B” embryo can still become an A+ baby.
- Embryo Growth Timeline:
- Day 1: Fertilized egg (zygote).
- Day 3: 6-8 cells, still tiny.
- Day 5: Blastocyst—ready for action!
Step 6: Embryo Transfer—Move-In Day
Time to put the embryo where it belongs—back in the uterus. This is the home stretch!
The Core Scoop
Using a thin catheter, the doctor slides the embryo into your uterus. It’s quick, no sedation needed, and you’re awake the whole time. Then, you wait to see if it “sticks.”
The Untold Stories
You’re lying there, legs up, with a full bladder (yep, it helps the ultrasound). Some clinics play music—one couple got “Sweet Child O’ Mine” during theirs! Afterward, people treat themselves gently, like royalty—think bubble baths or ordering takeout.
Science Says
A 2024 report from Human Reproduction found that frozen embryo transfers (where embryos are frozen first, then thawed later) have a 5-10% higher success rate than fresh ones. Cool, huh?
Your To-Do List
- ✔️ Stay calm: It’s normal to feel nervous, but stress won’t ruin it.
- ❌ Don’t over-rest: Bed rest isn’t required—move around lightly.
- Transfer Day Prep:
- Drink water an hour before (full bladder = better view).
- Wear comfy clothes.
- Bring a playlist if your clinic allows.
Step 7: The Two-Week Wait—Nail-Biting Time
After transfer, you wait about 9-14 days to find out if you’re pregnant. This is the longest short time ever.
The Core Scoop
Your embryo needs to implant in the uterus lining. You’ll take progesterone (a hormone) to help it along, then get a blood test to check for pregnancy.
The Juicy Details
This wait drives people wild. Some swear they feel “implantation twinges” (science says maybe, maybe not). Others pick up quirky habits—like one woman who knit a scarf for every day of the wait. Online, folks trade “symptom-spotting” stories: sore boobs, cramps, or cravings.
Expert Take
Dr. Sarah Lopez, a fertility counselor, notes, “The two-week wait is a mental marathon. Finding a small, joyful distraction can make all the difference.”
Survival Guide
- ✔️ Plan a project: Paint a room, binge a series—keep busy!
- ❌ Don’t test early: Home pregnancy tests can lie before the blood test.
- Symptom Decoder:
- Tiredness? Could be progesterone, not pregnancy.
- Nausea? Maybe a sign—or just nerves.
What Affects IVF Success? The Nitty-Gritty
Not every IVF cycle works, and that’s tough to hear. Let’s break down what plays a role.
Age: The Big One
Younger women (under 35) have a 40-50% chance per cycle, says the CDC’s 2023 ART Report. Over 40? It drops to 10-20%. Why? Egg quality fades with time.
Lifestyle Secrets
Smoking cuts success by 30%, per a 2022 Fertility Research study. Stress, diet, and even too much caffeine can nudge the odds, too.
Embryo Quality
Top-grade embryos (A or B) implant better. New tech, like AI picking embryos, is boosting rates by 15%, per a 2024 Science Daily article.
Tips to Tilt the Scales
- ✔️ Eat smart: Load up on veggies, nuts, and fish—think Mediterranean diet.
- ❌ Skip the vices: No cigs, less booze, and cut coffee to one cup.
| Factor | Boosts Success | Lowers Success |
|---|---|---|
| Age | Under 35 | Over 40 |
| Lifestyle | Healthy diet | Smoking |
| Embryo Grade | A or B | C or lower |
The Emotional Side—What No One Prepares You For
IVF isn’t just physical—it’s a heart-and-soul journey.
The Highs and Lows
You might feel hope one day, despair the next. One couple I know celebrated every step with a mini dance party—until a negative test hit. Then, they cried over pizza.
Hobbies That Help
People get creative: painting, yoga, even building Lego sets. It’s about finding your “thing” to stay grounded.
Expert Wisdom
Dr. Mark Evans, a psychologist, says, “IVF tests resilience. Small rituals—like a daily walk—can anchor you through the chaos.”
Coping Hacks
- ✔️ Talk it out: Friends, a therapist, or online groups—don’t bottle it up.
- ❌ Don’t isolate: Hiding hurts more than sharing.
Costs and Real Talk—What’s the Damage?
IVF isn’t cheap, and that’s a biggie for most folks.
The Numbers
One cycle averages $15,000-$20,000 in the U.S., per the 2024 Fertility Clinic Survey. Add meds, tests, and freezing embryos, and it can hit $30,000.
Hidden Costs
Time off work, travel to clinics, even therapy—those add up. Some cut corners by picking clinics with payment plans or grants.
Money-Saving Ideas
- ✔️ Check insurance: Some states cover parts of IVF—ask!
- ❌ Don’t skimp on quality: A cheaper clinic might mean lower success rates.
What’s Next? The Future of IVF
IVF’s evolving fast, and the future’s wild.
Cool New Tech
- In vitro gametogenesis (IVG): Making eggs or sperm from skin cells—still experimental, but mind-blowing.
- AI embryo selection: Already here, picking winners with crazy accuracy.
Latest Stats
A 2025 Reproductive Sciences preview predicts IVF could help 10% of babies worldwide by 2030 if costs drop.
Get Ahead
- ✔️ Stay curious: Follow fertility blogs for updates.
- ❌ Don’t jump on hype: New stuff needs testing—wait for proof.
Wrapping It Up—Your IVF Adventure Awaits
The IVF process is a marathon, not a sprint. From egg-boosting shots to the nail-biting two-week wait, it’s a mix of science, hope, and a dash of quirks—like knitting for luck or dreaming up embryo nicknames. It’s not always easy, but it’s a path millions have walked to hold their little ones. Armed with this guide, you’ve got the scoop on every step, plus some insider tricks to make it your own.
Let’s Chat!
What’s your take on IVF? Got a hobby that’s kept you sane through tough waits? Drop a comment below—I’d love to hear your story or answer your questions!