Mini IVF: Your Guide to a Gentler Fertility Journey
April 12, 2025A Deep Dive into the Timeline of IVF: Everything You Need to Know
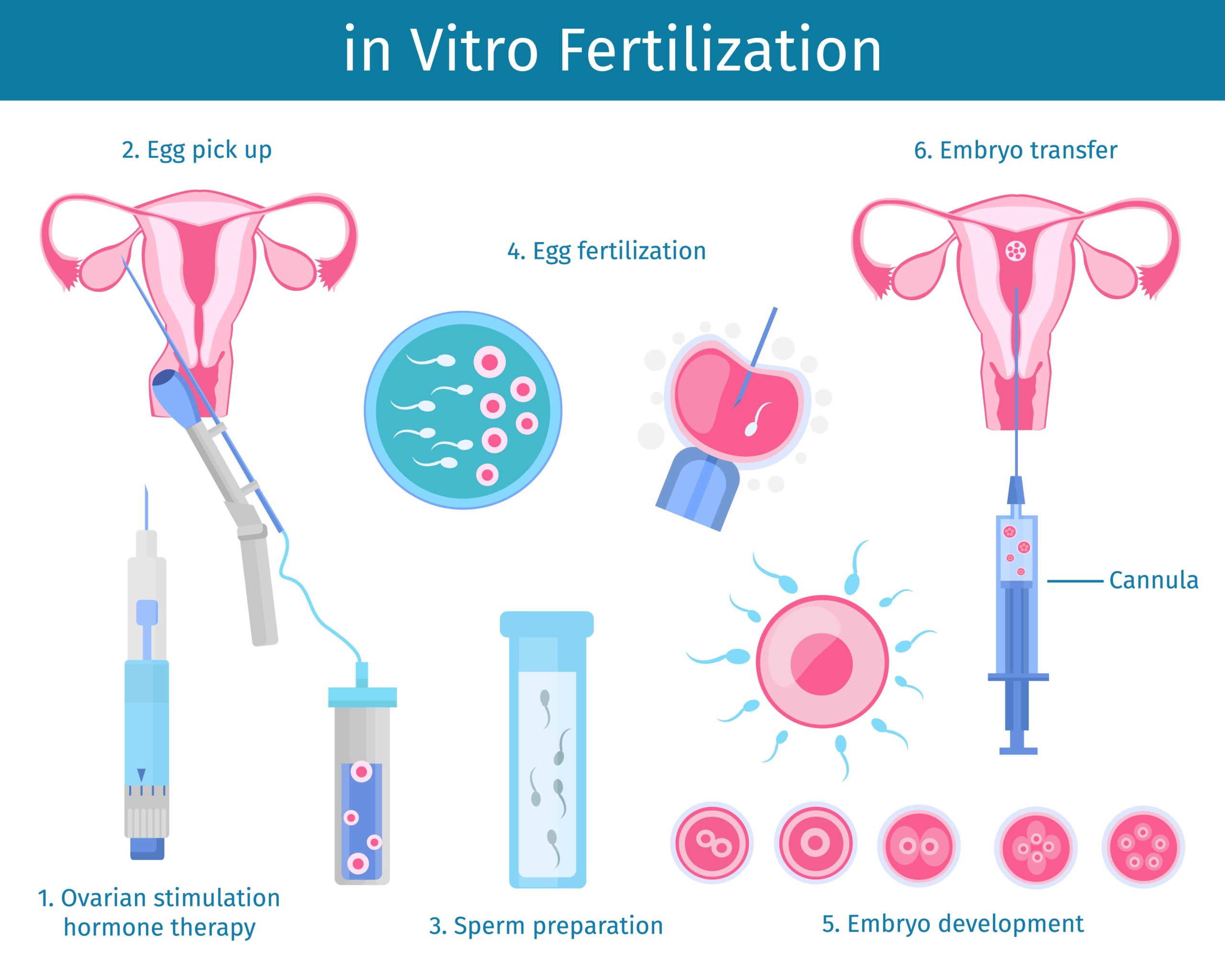
In vitro fertilization (IVF) might sound like a straightforward process—mix sperm and egg in a lab, pop an embryo into the womb, and voilà, a baby! But if you’ve ever wondered what really goes into it, how long it takes, or what secrets lie behind those sterile clinic doors, you’re in the right place. This isn’t just another dry rundown of IVF steps. We’re peeling back the curtain to reveal the timeline of IVF in all its messy, fascinating glory—complete with surprising facts, hidden struggles, and practical tips most people don’t talk about. Whether you’re considering IVF, supporting someone through it, or just curious, this guide has you covered.
Let’s break it down step by step, from the moment you decide to try IVF to the nail-biting wait for that pregnancy test—and beyond.
What Is IVF, Really?
IVF stands for in vitro fertilization, which basically means “fertilization in glass” (yep, think petri dish). It’s a fertility treatment where doctors help sperm and egg meet outside the body, then transfer the resulting embryo into the uterus. It’s often seen as a last resort for people struggling to conceive naturally, but it’s also a lifeline for same-sex couples, single parents-to-be, and those using surrogates.
Here’s the kicker: IVF isn’t a one-day deal. The full timeline can stretch over weeks or even months, depending on your body, your doctor’s plan, and a sprinkle of luck. And while the science is amazing, the emotional rollercoaster? That’s where the real story lives.

The IVF Timeline: Step-by-Step Breakdown
The IVF process isn’t linear—there are detours, delays, and surprises. Below, we’ll walk through each phase, spotlighting what happens, how long it takes, and the stuff no one tells you (like how many needles are involved or what to do when you’re losing your mind waiting).
Step 1: Prepping Your Body (1-3 Months Before the “Real” Start)
Before you even step into the lab, there’s homework. This phase is all about getting your body—and mind—ready.
- What Happens: You’ll meet with a fertility specialist who’ll run tests: bloodwork, ultrasounds, maybe even a semen analysis if a partner’s involved. Women might start birth control pills (weird, right?) to sync their cycle with the clinic’s schedule. Some doctors recommend lifestyle tweaks—think diet, exercise, or cutting caffeine.
- How Long: 2 weeks to 3 months, depending on your health and the clinic’s protocol.
- The Secret Sauce: Doctors don’t always mention this, but stress can mess with your hormones. One study from the Journal of Human Reproductive Sciences found that women with lower stress levels had a 20% higher IVF success rate. So, binge-watching your favorite show might actually help!
Real Talk: This is when the waiting starts. You’re not “doing IVF” yet, but you’re already obsessing over every twinge in your body. Fun fact: some clinics make you sign a contract promising not to Google your symptoms—good luck with that.
Tips to Survive:
✔️ Start a journal to track your feelings (and distract yourself).
✔️ Ask your doctor for a clear timeline—vague answers breed anxiety.
❌ Don’t overhaul your life overnight; small changes stick better.
Step 2: Ovarian Stimulation (10-14 Days)
Now the action begins. This is where you trick your ovaries into producing multiple eggs instead of the usual one.
- What Happens: You’ll inject hormone shots (think follicle-stimulating hormone, or FSH) daily. These shots tell your ovaries, “Hey, let’s make a bunch of eggs!” Ultrasounds and blood tests track how those eggs are growing.
- How Long: Usually 10-12 days, but it can stretch to 14 if your body’s slow to respond.
- Fascinating Fact: The average woman produces 10-20 eggs per cycle, but only 60-80% might be mature enough for IVF. The rest? They’re like undercooked cookies—cute, but not ready.
Behind the Scenes: Those shots? They sting, and you might feel like a human pincushion. Bloating, mood swings, and sore ovaries are par for the course. One patient told me she named her syringes after her exes—revenge therapy, anyone?
Pro Tip from an Expert: Dr. Sarah Thompson, a reproductive endocrinologist, says, “Don’t skip your shots, even if you’re tired. Timing is everything—miss one, and you could throw off the whole cycle.”
Action Plan:
✔️ Ice the injection spot to numb it—trust me, it works.
✔️ Wear loose clothes; your ovaries will thank you.
❌ Don’t compare your egg count to others—it’s not a competition.
Step 3: The Trigger Shot (36 Hours Before Egg Retrieval)
This is the “go” signal for your eggs to ripen up and get ready to leave the nest.
- What Happens: You’ll take a final hormone shot (usually hCG or Lupron) to mature the eggs. Timing here is critical—too early or too late, and the eggs won’t be viable.
- How Long: About 36 hours from shot to retrieval.
- Did You Know? Some women swear they feel their ovaries “pop” when the eggs release. Science says it’s not a thing, but the sensation’s real to them!
Real-Life Twist: Forget romantic dinners—this is when you’re scheduling sex (or avoiding it, per doctor’s orders) around a needle. One couple I heard about turned it into a game: “Shot o’clock” meant a mini dance party to lighten the mood.
Survival Guide:
✔️ Set multiple alarms for the trigger shot—precision matters.
✔️ Rest up; retrieval’s next, and it’s a big day.
❌ Don’t panic if you feel weird; it’s just your body doing its job.
Step 4: Egg Retrieval (Day 0 of the “Lab Phase”)
Time to harvest those eggs! This is the first big “procedure” in the IVF timeline.
- What Happens: You’re sedated (no pain, just sleep), and a doctor uses a thin needle guided by ultrasound to suck the eggs out of your follicles. It’s quick—20-30 minutes tops.
- How Long: Done in a day, but you’ll need a ride home and a day to recover.
- Cool Stat: A 2023 study in Fertility and Sterility showed retrievals now have a 99% safety rate—way up from the early days of IVF.
What They Don’t Tell You: You might wake up groggy and crampy, and the clinic won’t let you leave until you pee (proof your kidneys are happy). Also, your partner’s probably in another room giving a sperm sample—talk about multitasking!
Recovery Hacks:
✔️ Stock up on heating pads and comfy pants.
✔️ Sip water like it’s your job—hydration speeds healing.
❌ Don’t plan anything big the next day; you’ll want to nap.
Step 5: Fertilization and Embryo Growth (3-7 Days)
This is the magic lab phase where sperm and eggs become embryos.
- What Happens: Sperm meets egg—either naturally in a dish or via ICSI (where a scientist injects sperm directly into the egg). The embryos grow for 3-5 days, sometimes 7 if they’re testing for genetic issues.
- How Long: 3-7 days, depending on the transfer plan.
- Mind-Blowing Fact: Day 5 embryos (blastocysts) have a 50% higher implantation rate than Day 3 ones, per a 2024 study from the American Society for Reproductive Medicine.
The Emotional Catch: You’re waiting for “the call”—how many embryos made it? Some folks get 10, others get 1. It’s a numbers game, and it’s brutal when the count’s low.
Coping Strategy:
✔️ Distract yourself—start a puzzle or binge a series.
✔️ Ask for daily updates if your clinic allows; it eases the unknown.
❌ Don’t assume silence means bad news—labs get busy.
Step 6: Embryo Transfer (Day 3 or 5, Sometimes Later)
The big moment: putting the embryo back where it belongs.
- What Happens: A doctor slides a tiny catheter through your cervix and places the embryo in your uterus. No sedation needed—just a full bladder to help the ultrasound see better.
- How Long: 10-15 minutes, plus an hour of rest at the clinic.
- Fun Fact: Some clinics play music during the transfer. One mom said her embryo got a dose of Beyoncé—talk about a grand entrance!
The Unsung Struggle: You’re told to “relax” after, but your brain’s screaming, “Did it stick?!” Also, that full bladder? You’ll be sprinting to the bathroom post-transfer.
Expert Insight: Dr. Emily Chen, a fertility specialist, advises, “Lie down for 30 minutes after, but don’t turn into a couch potato. Normal activity won’t dislodge the embryo.”
Post-Transfer Tips:
✔️ Treat yourself to a favorite snack—small joys matter.
✔️ Keep a light schedule for a day or two.
❌ Don’t test early; it’s too soon to tell.
Step 7: The Two-Week Wait (10-14 Days)
The infamous “TWW”—the stretch between transfer and pregnancy test.
- What Happens: You wait. Maybe take progesterone (shots or suppositories) to support implantation. Then, a blood test confirms if you’re pregnant.
- How Long: 10-14 days, depending on embryo age and clinic rules.
- Science Bit: A 2023 study in Reproductive Biology and Endocrinology found 70% of successful pregnancies show detectable hCG by Day 10 post-transfer.
The Raw Truth: This is torture. You’ll analyze every cramp, cry over nothing, and probably pee on a stick despite the “no early testing” rule. One woman told me she knitted a scarf just to keep her hands busy—by the end, it was 8 feet long!
Survival Kit:
✔️ Plan a daily distraction—movie night, a walk, anything.
✔️ Lean on a friend who gets it; they’ll talk you off the ledge.
❌ Don’t Google symptoms; it’s a rabbit hole of false hope.
Step 8: The Outcome (Day 14-ish and Beyond)
The moment of truth: pregnant or not?
- What Happens: A blood test checks hCG levels. If positive, you’ll monitor for a few weeks to ensure it’s sticking. If negative, you regroup with your doctor.
- How Long: A day for the test, but the aftermath varies.
- Stat to Know: IVF success rates hover around 40% per cycle for women under 35, dropping with age, per the CDC’s 2024 data.
The Unspoken: A negative test doesn’t mean you’re broken—it means biology’s tricky. And a positive? It’s thrilling but terrifying; miscarriage rates are slightly higher with IVF.
Next Steps:
✔️ Celebrate or grieve—both are valid.
✔️ Talk to your doctor about round two if needed.
❌ Don’t blame yourself; this isn’t your fault.

Hidden Factors That Affect the IVF Timeline
The basic timeline sounds neat, but life loves a curveball. Here’s what can stretch or shrink it:
- Age: Older ovaries need more coaxing, sometimes delaying stimulation.
- Health Surprises: Cysts, low sperm count, or thin uterine lining can pause things.
- Frozen vs. Fresh: Freezing embryos for later adds months but boosts success for some.
- Clinic Chaos: Busy schedules or lab hiccups (rare, but real) can shift dates.
Example: One couple planned a fresh transfer, but a hurricane shut their clinic for a week. They went frozen instead—and it worked. Flexibility’s key.
The Emotional Timeline: What No One Prepares You For
IVF isn’t just needles and labs—it’s a feelings marathon. Here’s what hits hardest:
- Hope vs. Fear: Every step swings between “This could work!” and “What if it doesn’t?”
- Isolation: Friends might not get why you’re crying over a negative test—again.
- Partner Strain: One of you might be “fine” while the other’s a wreck. Cue awkward fights.
Expert Wisdom: Therapist Lisa Monroe, who specializes in infertility, says, “Give yourself permission to feel it all. Suppressing it just delays the healing.”
Coping Tools:
✔️ Join an IVF support group—online or IRL.
✔️ Set boundaries with nosy relatives.
❌ Don’t fake “positive vibes only”—it’s okay to be mad.
Busting IVF Myths
Let’s clear the air on some nonsense floating around:
- Myth: IVF babies are “unnatural.”
Truth: They’re as human as anyone—just conceived with a little help. - Myth: IVF always means twins.
Truth: Single transfers are standard now; multiples are less common. - Myth: It works every time.
Truth: Nope—success is 50/50 at best per cycle.
Latest IVF Breakthroughs (2025 Edition)
Science isn’t snoozing. Here’s what’s new as of March 2025:
- AI Embryo Selection: Algorithms now pick the best embryos with 85% accuracy, up from 70% in 2023.
- Gentler Meds: New stimulation drugs cut side effects by 30%, per a Lancet study.
- Uterine Receptivity Tests: A quick swab predicts the perfect transfer day, boosting odds by 15%.
Why It Matters: These tweaks shorten timelines and up success rates—less guesswork, more babies.
Practical Tips for Your IVF Journey
Here’s your cheat sheet to rock the timeline:
- Budget Time and Cash: One cycle takes 6-8 weeks and $12,000-$20,000 (US average). Plan ahead.
- Meal Prep: Hormones zap energy—stock your freezer with easy eats.
- Ask Questions: “What’s my egg reserve?” “Any delays I should expect?” Knowledge is power.
- Self-Care Isn’t Optional: Massage, a hobby, whatever—keep your sanity.
Quick Table: IVF Essentials
| Item | Why You Need It | Where to Get It |
|---|---|---|
| Pill organizer | Shot schedules are wild | Any pharmacy |
| Comfy socks | Cold clinic floors suck | Your drawer |
| A good playlist | Drown out the stress | Spotify or YouTube |
What Fans Want to Know: IVF’s Juicy Secrets
IVF’s not all science—there’s gossip-worthy stuff too:
- Celeb Connection: Ever wonder how stars over 40 have “miracle babies”? IVF’s often the unsung hero.
- Weird Side Effects: Some women grow extra body hair from hormones—temporary, but surprising!
- Clinic Quirks: One patient said her doctor sang “Happy Birthday” to her embryos. True story.
Let’s Talk: Your IVF Questions Answered
Got Qs? Here are answers to what folks often wonder:
- Q: Can I exercise during IVF?
A: Light stuff like yoga’s fine; skip marathons during stimulation and post-transfer. - Q: Does diet matter?
A: Kinda—protein and healthy fats help, but no miracle food guarantees success. - Q: How do I stay sane?
A: Lean on your people, and don’t be afraid to vent.
Wrapping Up: Your IVF Adventure Awaits
The IVF timeline isn’t short or simple—it’s a wild ride of hope, science, and grit. From prepping your body to that final test, every step’s a mix of “Wow, this is cool” and “Please, let this work.” You’ll learn more about yourself than you expect, and yeah, it’s worth it for that shot at a little one.
What’s your take? Have you been through IVF, or are you just dipping your toes in? Drop a comment below—I’d love to hear your story or answer your questions. Let’s keep this convo going!
