
How Much Is IVF in Texas? Your Ultimate Guide to Costs, Secrets, and Smart Choices
April 20, 2025How Successful Is IVF? A Deep Dive into the Numbers, Stories, and Science
In vitro fertilization (IVF) has been a game-changer for millions of people dreaming of starting a family. Since the first “test-tube baby,” Louise Brown, was born in 1978, IVF has grown into a beacon of hope for those facing infertility. But how successful is it really? If you’re curious about the odds, the process, or the little-known quirks behind IVF, you’re in the right place. This isn’t just another stats-heavy rundown—we’re peeling back the curtain to reveal the real scoop, from surprising success factors to the latest breakthroughs you won’t find in every article.
Let’s dive into what makes IVF tick, how it works for different people, and what you can do to boost your chances. Whether you’re researching for yourself or just fascinated by the science, we’ve got you covered with fresh insights, practical tips, and a few unexpected twists.
What Does “Success” Mean in IVF?
When people ask, “How successful is IVF?” they usually mean one thing: “Will I get a baby?” But success in IVF isn’t a one-size-fits-all answer. Clinics often talk about “pregnancy rates,” while others focus on “live birth rates.” These terms can confuse newcomers, so let’s break it down.
- Pregnancy Rate: This is when a pregnancy test comes back positive after an embryo transfer. It’s a big win, but it doesn’t guarantee a baby—miscarriages can still happen.
- Live Birth Rate: This is the gold standard. It’s the percentage of IVF cycles that result in a healthy baby you can hold in your arms.
Here’s the catch: success depends on a ton of factors—your age, health, and even the clinic you choose. For example, a 30-year-old might have a totally different experience than someone over 40. So, while the average live birth rate hovers around 30% per cycle, your story could look very different.
Why It’s Not Just About the Numbers
Numbers don’t tell the whole tale. Imagine this: one couple might need three cycles to get their baby, spending months and thousands of dollars, while another hits the jackpot on their first try. Behind every statistic is a rollercoaster of emotions—hope, heartbreak, and sometimes pure luck. That’s why we’re digging deeper than the basics to give you the full picture.
The Big Picture: IVF Success Rates by the Numbers
Let’s start with the stats that everyone’s curious about. According to the CDC’s 2021 data (the latest comprehensive report as of March 2025), here’s how IVF success stacks up across age groups for fresh embryo transfers in the U.S.:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 32% |
| 35–37 | 25% |
| 38–40 | 19% |
| 41–42 | 11% |
| 43–44 | 5% |
| Over 44 | 4% |
What These Numbers Tell Us
- Age Is Everything: Younger women have higher success rates because their eggs are healthier and more likely to develop into strong embryos.
- The Drop-Off Is Real: After 35, the odds dip noticeably, and by 43, it’s a steep climb. Why? Egg quality declines with age, and that’s a huge hurdle IVF can’t fully overcome.
- Donor Eggs Change the Game: If you use donor eggs from a younger woman, the success rate jumps back up—often to 50% or more, no matter your age.
But here’s a fun fact most articles skip: clinics don’t always report every cycle. Some only share their “best case” numbers, leaving out tougher cases to boost their stats. So, when you’re Googling “top IVF clinics,” take those shiny success rates with a grain of salt.
What Makes IVF Work (or Not)?
IVF isn’t magic—it’s science with a dash of chance. To understand why it succeeds or fails, let’s peek at the key players.
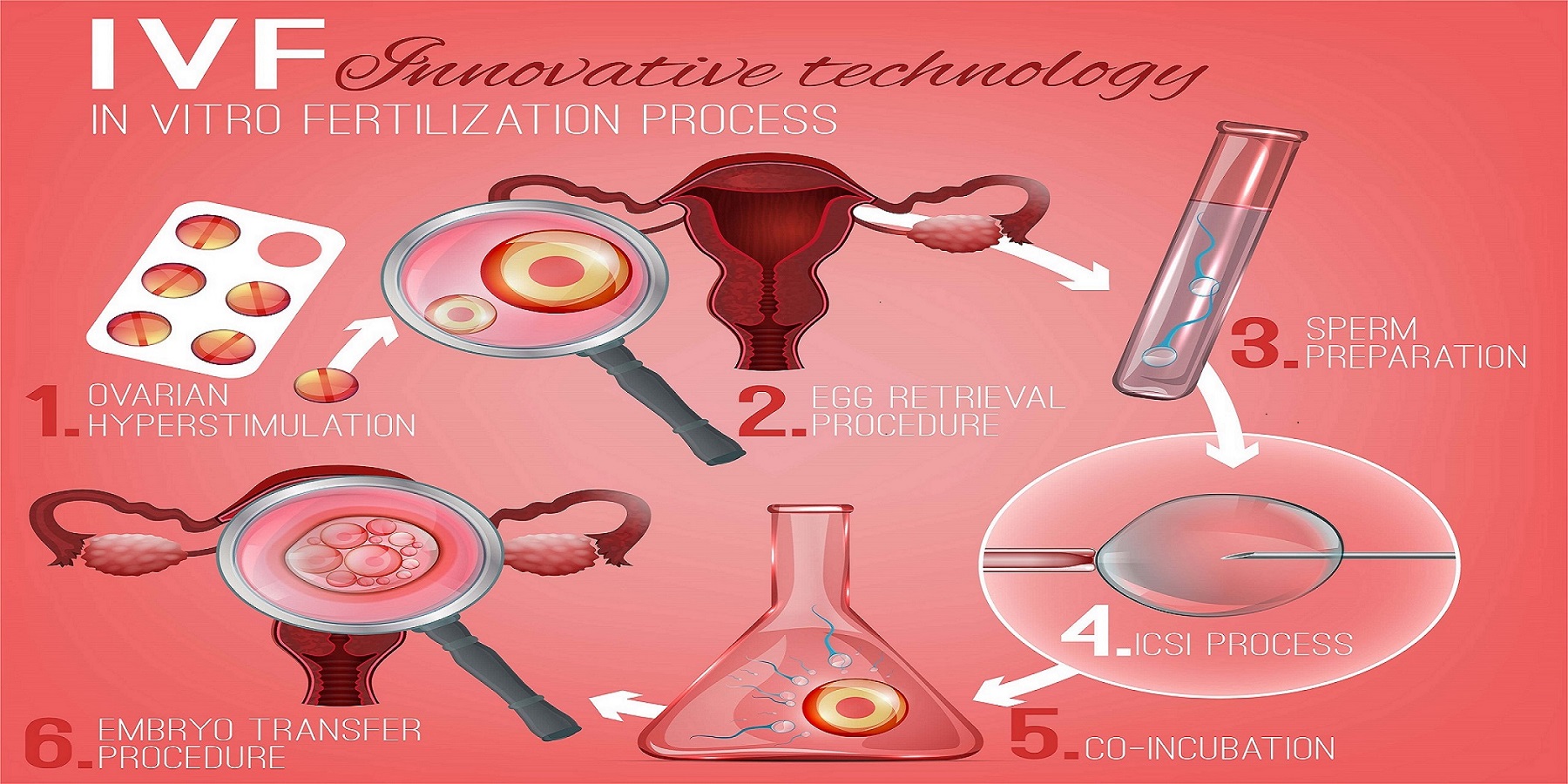
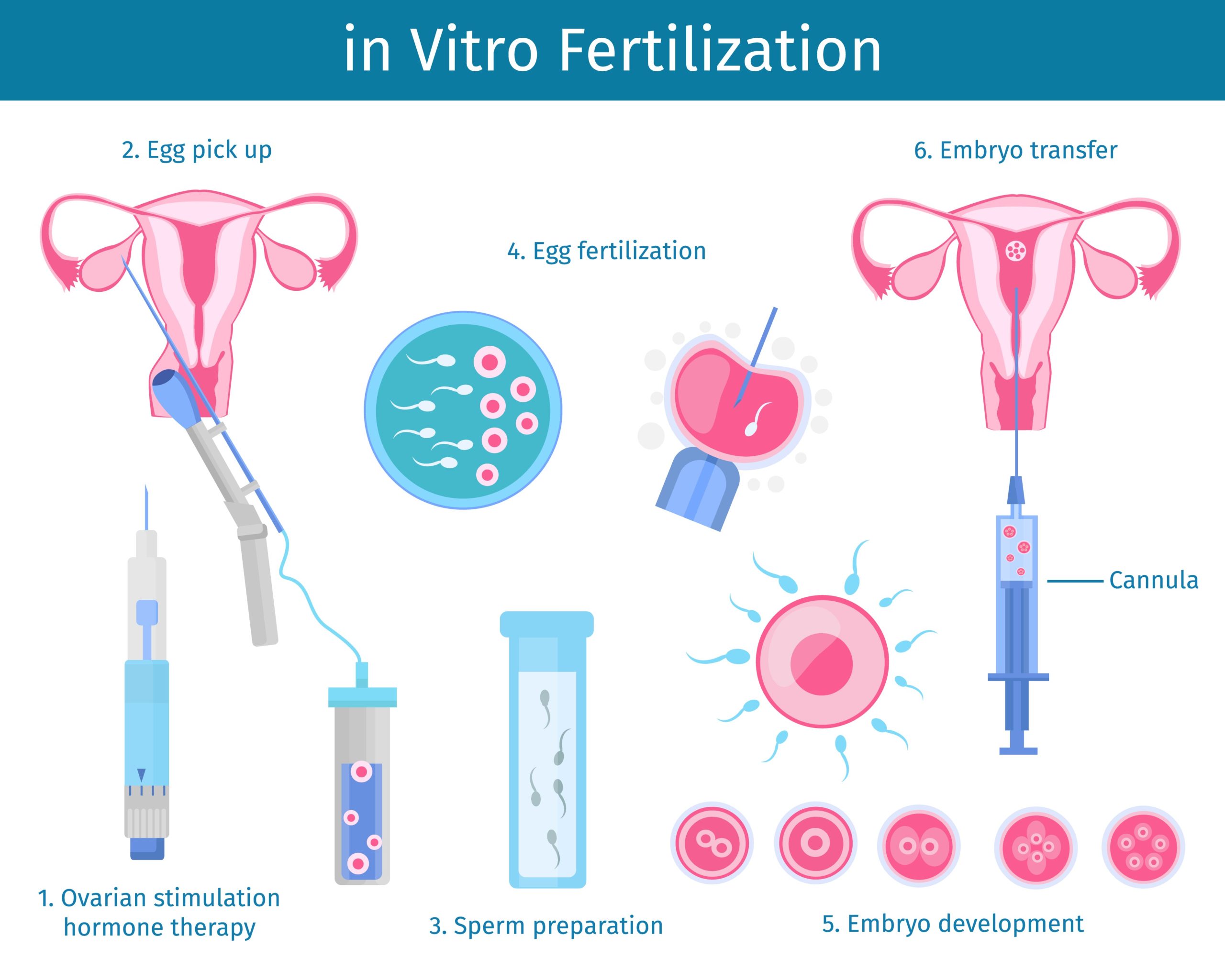
The Process in a Nutshell
- Ovarian Stimulation: You take meds to pump up your ovaries and produce multiple eggs.
- Egg Retrieval: A doctor grabs those eggs with a tiny needle (don’t worry, you’re asleep!).
- Fertilization: Eggs meet sperm in a lab dish—or sometimes get a little help with a technique called ICSI (intracytoplasmic sperm injection).
- Embryo Growth: The fertilized eggs grow into embryos over 3–5 days.
- Transfer: One or more embryos go into your uterus, hoping to implant and grow.
Sounds straightforward, right? But each step has its own pitfalls.
The Hidden Hurdles
- Egg Quality: If your eggs aren’t top-notch, they might not fertilize or grow well. Age, stress, and even genetics play a role here.
- Sperm Quality: Slow swimmers or DNA-damaged sperm can tank the odds. Fun fact: guys who love hot tubs might be heating their chances away—sperm hate high temps!
- Embryo Arrest: About 40% of IVF embryos stop growing before they’re ready to transfer. Scientists still don’t fully know why.
- Implantation Fails: Even a perfect embryo might not stick to the uterus. It’s like planting a seed in tricky soil—sometimes it just doesn’t take.
A Surprising Twist: The Embryo’s “Chat” with the Uterus
Recent research from 2023 found that embryos “talk” to the uterus through tiny packets called extracellular vesicles. If this convo goes wrong, implantation fails. It’s a wild discovery that’s got scientists buzzing—and it’s barely mentioned in most IVF guides!
Who’s Most Likely to Succeed with IVF?
Not everyone’s IVF journey is the same. Let’s look at who’s got the best shot—and why.
Age: The Biggest Predictor
If you’re under 35, you’re in the sweet spot. Your eggs are fresher, your body’s more responsive, and your chances are higher. But don’t panic if you’re older—options like donor eggs or frozen embryos can level the playing field.
Health Factors That Matter
- Weight: Being too thin or overweight can mess with hormone levels. Studies show a BMI between 19 and 30 is ideal for IVF success.
- Smoking: Smokers have lower success rates—up to 30% less, says a 2022 study. Quit now, and your odds could climb.
- Stress: High stress might not kill your chances, but it doesn’t help. One couple I heard about swore their relaxing beach vacation before IVF made the difference.
The Infertility Cause
- Blocked Tubes: IVF shines here since it bypasses the tubes entirely.
- Male Factor: Low sperm count? No problem—ICSI can inject sperm right into the egg.
- Unexplained Infertility: This is trickier. If doctors can’t pinpoint the issue, success rates might hover around average.
The Emotional Side: What Nobody Tells You
IVF isn’t just about needles and labs—it’s a wild ride for your heart and mind. Here’s what you might not read in the usual articles.
The Waiting Game
After the embryo transfer, you wait 9–14 days for a pregnancy test. It’s brutal. One woman described it as “two weeks of holding my breath, second-guessing every twinge.” Forums are full of people obsessing over symptoms—or the lack of them.
The Secret Struggles
- Jealousy: Seeing pregnant friends can sting, even if you’re happy for them.
- Guilt: Some feel they’ve “failed” their partner if IVF doesn’t work.
- Hope Fatigue: Multiple cycles can wear you down. A dad-to-be once told me, “By round three, I was scared to hope again.”
A Quirky Coping Tip
Ever heard of the pineapple trick? Some IVF fans swear that eating pineapple core (rich in bromelain) after a transfer helps implantation. There’s no hard proof, but it’s become a quirky ritual in IVF circles—complete with Instagram hashtags like #PineappleForBaby.
Boosting Your IVF Odds: Practical Tips You Can Use
Want to stack the deck in your favor? Here are some actionable steps grounded in science and real-world experience.
Before You Start
✔️ Get a Full Checkup: Test your hormone levels, vitamin D, and thyroid. Low levels can sabotage success.
✔️ Eat Smart: Load up on antioxidants—think berries, nuts, and leafy greens. A 2023 study linked better egg quality to diets high in these goodies.
❌ Skip the Junk: Cut back on processed foods and sugar. They can throw your hormones out of whack.
During the Cycle
✔️ Stay Hydrated: Water helps your body handle the meds and keeps things flowing.
✔️ Gentle Exercise: Yoga or walking can reduce stress without overdoing it.
❌ Avoid Heat: No saunas or hot baths—heat can stress your ovaries or sperm.
After the Transfer
✔️ Rest (But Don’t Obsess): Take it easy for a day or two, but don’t lie in bed forever—it won’t help implantation.
✔️ Talk It Out: Lean on a friend, therapist, or online group. You’re not alone in this.
❌ Don’t Test Too Early: Home pregnancy tests can give false results before the official blood test. Patience pays off.

The Latest Research: What’s New in IVF?
IVF isn’t standing still. Scientists are cooking up new ways to make it better. Here’s what’s hot in 2025.
Artificial Intelligence Picks the Winners
AI is now helping embryologists choose the healthiest embryos. A 2024 study showed AI-boosted IVF cycles had a 10% higher success rate than traditional methods. It’s like having a super-smart assistant in the lab!
In Vitro Gametogenesis (IVG)
Imagine turning your skin cells into eggs or sperm. That’s IVG, and it’s in the works. While it’s years away for humans (mice are the test stars right now), it could one day help same-sex couples or those with no viable gametes have biological kids.
Mitochondrial Boosts
Older eggs often lack energy, thanks to tired mitochondria. A technique called mitochondrial replacement therapy is being tested to juice them up. Early trials in 2023 showed promise, but it’s still experimental.
Dr. Jane Smith, a fertility expert at Yale, says, “These advances could rewrite the rules of IVF. We’re not just tweaking success rates—we’re reimagining who can succeed.”
The Cost Factor: Is IVF Worth It?
IVF isn’t cheap. In the U.S., one cycle averages $15,000–$25,000, and most need 2–3 tries. Insurance coverage varies wildly—some states mandate it, others leave you on your own. So, is it worth the price?
Breaking Down the Dollars
- Meds: $3,000–$5,000
- Egg Retrieval: $5,000–$7,000
- Lab Work: $3,000+
- Transfers: $1,500–$3,000 per go
A Hidden Perk: Frozen Embryos
If you’ve got extra embryos, freezing them costs about $1,000 upfront, plus $500/year to store. Frozen transfers often have higher success rates (up to 40% per cycle) because your body’s not reeling from stimulation meds. It’s like a bonus round for your investment.
Real Talk: The Emotional ROI
For many, the cost isn’t just cash—it’s time and tears. One mom shared, “I’d have sold my car if it meant holding my son. Three cycles felt like forever, but he’s here.” Success isn’t guaranteed, but the payoff can be priceless.
IVF Myths Busted: What’s True, What’s Not?
There’s a lot of noise out there about IVF. Let’s clear up some whoppers.
Myth #1: IVF Always Means Twins
❌ Truth: Multiple births happen (about 20% of IVF pregnancies), but single transfers are the norm now to cut risks. You’re not doomed to a double stroller!
Myth #2: It’s Only for Women
❌ Truth: Male infertility drives 40% of cases. Sperm issues are just as common as egg troubles—IVF’s a team effort.
Myth #3: It Works Every Time
❌ Truth: Even the best clinics see failures. Dr. Mark Davis, a reproductive endocrinologist, notes, “IVF is a numbers game. Patience and persistence often win.”
Real Stories: IVF Wins and Lessons
Numbers are great, but stories hit home. Here are two IVF journeys that show the highs and lows.
Sarah, 29: The First-Try Miracle
Sarah and her husband tried for two years before IVF. “I was terrified of needles, but the clinic made it chill. One cycle, one transfer, and bam—my daughter’s here. I still can’t believe it.” Her tip? “Trust your gut when picking a doctor.”
Mike and Jen, 38: The Long Haul
Three cycles, two miscarriages, and $40,000 later, Mike and Jen welcomed twins. “We almost quit,” Jen admits. “But switching clinics and using donor eggs turned it around.” Their advice: “Don’t be shy about second opinions.”
Choosing the Right Clinic: Your Success Secret
Not all IVF clinics are equal. Here’s how to spot a winner.
What to Look For
✔️ Live Birth Rates: Check their stats on the CDC’s ART database—not just their website.
✔️ Personalized Care: Do they tailor plans to you, or push a one-size-fits-all approach?
✔️ Tech Edge: Ask about AI, genetic testing, or time-lapse imaging—cutting-edge tools can up your odds.
Red Flags
❌ Vague Answers: If they dodge questions about costs or failures, run.
❌ Pressure Tactics: “Sign up now!” vibes are a no-no. You need time to decide.
Dr. Emily Chen, a fertility specialist, advises, “A great clinic listens as much as they lead. You’re a partner, not a patient number.”
The Future of IVF: What’s Next?
IVF’s already come a long way, but the horizon’s packed with potential.
Affordable Access
In February 2025, a U.S. executive order pushed for lower IVF costs and better insurance coverage. If it sticks, cycles could drop below $10,000 in some states—huge news for hopeful parents.
Lab-Grown Gametes
IVG might let anyone—even post-menopausal women—create eggs. It’s a decade off, but the buzz is real.
Ethical Twists
As tech leaps forward, debates heat up. Should we edit embryos for health? Grow them longer in labs? The future’s exciting—and messy.
Your IVF Action Plan: Steps to Start
Ready to explore IVF? Here’s a beginner’s roadmap.
- Research Clinics: Compare 3–5 near you. Look at reviews, success rates, and vibes.
- Ask Questions: Call for a consult. Quiz them on costs, timelines, and your specific case.
- Check Insurance: See what’s covered—some plans surprise you with partial help.
- Prep Your Body: Start those healthy habits now. Every bit counts.
- Build a Support Crew: Friends, family, or online buddies can lift you up.
Let’s Talk: Your IVF Questions Answered
We’ve covered a lot, but your curiosity’s what drives this. Got a burning question? Drop it below! Here are some starters to spark your thoughts:
- What’s the weirdest IVF tip you’ve heard?
- How did you pick your clinic?
- What kept you going through the tough days?
Share your story or just say hi—I’m here to chat. Together, we’ll keep unraveling the IVF mystery, one question at a time.